Evaluating Serviceability of Healthcare Servicescapes: Service Design Perspective
Seunghae Lee
Purdue University, West Lafayette, U.S.A.
The recent interest in and efforts to improve healthcare facility users’ experiences has led to design research projects that have studied the role of the environment in the healing process (Delvin, 2003). The healthcare industry now recognizes that servicescapes are important resources for the impact they can have on customers (Fottler, Ford, Roberts, & Ford, 2000). Healthcare facilities that have developed business strategies that offer patient-centered care have employed a range of research approaches such as servicescapes, design thinking, and service design. This study examines the design of ambulatory healthcare from a service design perspective. It focuses on healthcare facilities as servicescapes and builds up a conceptual framework that outlines servicescape features in healthcare facilities, perceived servicescapes, users’ emotional and physiological statuses, and attitudes towards the healthcare. An exploratory case study has been conducted for a local outpatient healthcare facility with a field survey, structured interviews, and a questionnaire survey. Based on results from the structured interviews, the questionnaire tool was developed to test the research framework. Findings from statistical analyses showed that servicescape features can be categorized into the two factors of ambient conditions and serviceability, and that these factors are related to satisfaction with the facility, perceived quality of care, and approach behavior.
Keywords – Healthcare Design, Servicescape, Serviceability, Service Design.
Relevance to Design Practice – This study with service design approaches to healthcare servicescapes suggests a conceptual framework based on the exploratory case study to help designers who are interested in patient-centered healthcare design.
Citation: Lee, S. (2011). Evaluating serviceability of healthcare servicescapes: Service design perspective.International Journal of Design, 5(2), 61-71.
Received November 1, 2010; Accepted April 30, 2011; Published August 15, 2011.
Copyright: © 2011 Lee. Copyright for this article is retained by the author, with first publication rights granted to the International Journal of Design. All journal content, except where otherwise noted, is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 2.5 License. By virtue of their appearance in this open-access journal, articles are free to use, with proper attribution, in educational and other non-commercial settings.
Corresponding Author:Lee30@purdue.edu
Seunghae Lee is an Assistant Professor at Purdue University. She has Ph.D. from Michigan State University in Facilities Management & Design. Her current research focus is physical environmental aspects and their impacts on healthcare facility users. Before she joined Purdue University she has taught at California State University at Northridge for three years. She holds certifications from the National Council for Interior Design Qualification in the U.S. and South Korea. She is a Leadership in Energy and Environmental Design (LEED) Accredited Professional.
Introduction
For the last two decades, the healthcare industry has gone through changes in healthcare service deliveries. These changes are a response to: higher service expectations from patients, ever-advancing technology, greater access to health information through the internet and the digital media, and a holistic approach to health and well-being concerns (Francis, 2010). In this competitive healthcare market with growing patient consumerism, it is important for healthcare providers to understand what patients and families experience in their facilities, how they perceive healthcare service quality, and what impacts those perceptions in order to satisfy and exceed patients’ wants and needs. In 2001, the Institute of Medicine (IOM) established six aims for improving healthcare quality. They are to be: safe, effective, patient-centered, timely, efficient, and equitable (IOM, 2001). Of all these aims, patient-centered healthcare has been a driving force for healthcare servicescape design. The healthcare industry has recognized the importance of servicescapes, or the physical environments of the organization, in shaping the service experience of its patients and families. They have drawn from the service provision of other industries such as restaurants and hotels to focus on customers as guests (Fottler, Ford, Roberts, & Ford, 2000).
The concept of patient-centered care is also tied closely to that of service design: to develop service encounters that are useful, usable, and desirable from the client’s perspective (Moritz, 2005). Parasuraman, Zeithaml, and Berry (1988) suggested a measurement tool to assess consumer perceptions with service quality (called SERVQUAL), and it has been popularly used in marketing research ever since. The tool is composed of five dimensions of service quality that include tangibles, reliability, responsiveness, assurance, and empathy. This composition of dimensions for service quality measurement shows that tangibles such as physical environments and equipment are crucial for consumer perceptions, although the service itself is intangible. Servicescapes are also tangible service qualities from which consumers develop perceptions about the service provider and, thus, are important components of service design that the service provider needs to evaluate for impact on consumer satisfaction in regard to quality of service. Healthcare providers should also consider the impact that the physical environment can have on encouraging or discouraging certain behaviors and emotions (Carpman & Grant, 1993) and the positive effect they can have in the healing process (Fottler et al., 2000).
The healthcare industry has gone through constant expansion since the 1960s. For the last twenty years, its transformation has focused more on internal reconstruction rather than building new facilities or additions to old facilities, with the exception of ambulatory healthcare facilities (Verderber & Fine, 2000). Some of the services that previously were offered only at large hospitals are now provided in specialty facilities such as outpatient surgery, diagnostic and testing, and free-standing urgent care centers (Carpman & Grant, 1993). The percentage of ambulatory healthcare service establishments in the U.S. reached 87.3 in 2008 (Bureau of Statistics in the U.S. Department of Labor, 2010). The growth in ambulatory healthcare services is reflected in the change in the International Building Codes (IBC) 2009: sections for “ambulatory health care” occupancy to enhance occupant safety were added (International Code Council, 2009). Despite this growth trend in ambulatory healthcare facilities, there is still very little research that has been undertaken for their service design.
This study focuses on ambulatory healthcare servicescapes from a service design perspective. Currently, studies on healthcare servicescapes examine perceived physical conditions of the facility, focusing on cleanliness and attractiveness and their relations to perceived quality of care and approach behaviors such as willingness to return and willingness to recommend. However, for healthcare providers and designers to understand patient needs and wants, they should know whether physical aspects of servicescapes serve patients properly. For example, although patients might consider a waiting area of an outpatient clinic aesthetically pleasing, the design of the waiting area will not serve the patient properly if the waiting area’s design makes it hard for patients to see or hear when a staff member calls the patient into the clinical area. Therefore, this study approaches servicescapes with service design perspectives that allow the exploration of patients’ experiences with the facility at each service encounter and the examination of the serviceability of servicescapes.
A conceptual framework was developed to delineate the relationship between servicescape features and customer responses. Previous studies and literature from multiple disciplines such as architectural design, marketing, and environmental psychology were examined to identify a comprehensive set of servicescape features in ambulatory healthcare and customer experiences including perceptions, emotions, satisfaction, and behaviors. In addition, an exploratory case study was conducted in an ambulatory healthcare facility to examine healthcare consumers’ experiences with healthcare servicescapes. The field survey and a total of 22 interviews have been conducted. Based on results from the interviews and observations, a survey tool was developed to measure consumer responses about serviceability and perceived physical conditions of servicescape features. One hundred seventy responses were gathered, and one hundred fifty-one responses were analyzed. The conceptual framework of healthcare servicescapes that has been developed in this study was tested with correlations and multiple regressions to investigate any causal relationship between factors. The moderating effect of customers’ physical status was assumed.
Service Design in Healthcare: Patient-Centered Care
The increases in the service industry’s development have transformed the service industry sector in many ways. The importance of design has been valued mainly in manufacturing industries that produce goods such as automotives, electronics, and packaged goods (Brown, 2008; Maffei, Mager, & Sangiorgi, 2005). However, the service industry has recently started to recognize and utilize designers’ abilities to enhance service development and delivery through design thinking. Designers’ abilities to think innovatively and their involvement in business development at the early stages are starting to make differences in the service sector. Meanwhile, service design was born as a discipline emerging from awareness that an economic view is dominant in the service sector and that there is a lack of intuitive and creative design culture (Maffei, Mager, & Sangiorgi, 2005). For successful business development, it needs to integrate both analytical and intuitive approaches. The analytical approach relies on quantitative information and logic-developing decisions from strategic approaches and data analysis. On the other hand, the intuitive approach is based on creative instincts and innovative ideas (Martin, 2009). To support business strategies effectively, service design integrates both analytical and intuitive approaches embracing other disciplines such as business, design, marketing, and human resources management. Service design is an interdisciplinary process that connects different areas of expertise. This integrative activity is critical in service design because methods, resources, skills, and experiences that various areas of experience offer are the keys to successful service design (Moritz, 2005).
The healthcare industry is one of the service industries that can benefit from the service design approach. As healthcare providers continue to focus on the importance of patient-centered care and seek to improve the quality of that care, they have started to implement important strategies that have been used in the guest services industry. One aspect of the focus on patient-centered care is the emphasis on consumers and their experiences which is also the core value of service design. Any industry that is interested in quality outcomes will value customer satisfaction, because satisfied customers are loyal customers. In the healthcare industry, the healthcare providers offer care, and it is assumed that consumers who are satisfied with their care will come back when they need care again (Otani, Waterman, Faulkner, Boslaugh, & Dunaga, 2010). Therefore, it is important to understand what patients and their families experience when they receive care from providers and to examine what contributes to healthcare service consumers’ satisfactions with care. Another reason why patient satisfaction is important in the healthcare industry is because patients’ experiences with and perceptions with care can be critical to healing or managing an illness (Institute of Medicine, 2001). In healthcare, environmental factors can affect moods and emotional states of patients, their families, and employees (Fottler et al., 2000). Although the healthcare design research area is still in its very early stages and needs to develop more of its methodologies, there have been many efforts to demonstrate the relationship between physical environmental factors and patient outcomes (Rubin, 1997). Some healthcare providers such as Kaiser Permanente and Mayo Clinic have implemented the practice of service design to enhance the quality of the experiences of patients and medical staff (Brown, 2008). Through the service design approach, healthcare providers can make innovations in healthcare delivery. IDEO, a design consulting firm, introduced a qualitative analysis of healthcare service using the Patient Journey Framework in an effort to translate the service system for the patient (Irwin, 2002). The framework helps researchers develop questions that patients may have at each stage as it follows patients’ movement in the facility.
Servicescape as a Service Design Component
Bitner (1992) coined the term “servicescape” to take the first step in developing a conceptual framework that integrates multiple disciplines and to study the impact of the physical environment of service organizations on consumers and employees. Since then, many studies from various disciplines examined the topic of servicescapes theoretically and empirically (Fottler et al., 2000; Lin, Leu, Breen, & Lin, 2008; Newman, 2007). Bitner (1992) suggested environmental dimensions such as ambient conditions, space/function, and signs/symbols/artifacts in her framework of environment/user relationships. This environment/user relationship framework depicts customers and employees perceiving various physical environmental factors, responding to them cognitively, emotionally, and physiologically, and being affected by their responses so as to alter their behaviors and social interactions with other customers and employees. Hutton and Richardson (1995) narrowed the topic to healthcare facilities and modified Bitner’s servicescape framework by combining it with Kotler’s atmospherics (1993). Atmospherics are physical characteristics and controllable physical environmental factors that affect consumer behaviors (Kotler, 1973).
While other service industries such as hospitality and retail have valued the role of the physical environment on customer satisfaction and retention and have put in an effort to provide a physical environment that exceeds the customer’s expectations, it was only recently that the healthcare industry recognized that servicescapes are important resources that can impact customers (Fottler et al., 2000). The recent interests in and efforts to improve healthcare facility users’ experiences led to implementations of design research that have studied diverse user groups to explore the role of the environment in the healing process (Arneill & Delvin, 2002). Topics in healthcare servicescape research have revolved around employee responses or inpatient healthcare facilities. To support the healthcare providers’ business strategy to provide patient-centered care with servicescapes, it is important to understand how patients experience and interact with physical environments. In other words, healthcare providers and designers need to evaluate how well healthcare servicescapes serve consumers. Most customers arrive at healthcare facilities with distressed, concerned, and anxious feelings, and the unfamiliar environment will only worsen their negative emotions. To create a servicescape that can satisfy customers’ needs for comfort, convenience, safety, security, privacy, and support, healthcare providers need to understand which servicescape features impact customer satisfaction and behavior and how. Most previous studies on healthcare facilities focused on the relationship between patients’ perceptions with the physical environmental factors of servicescapes, their perceptions with the quality of care, and their willingness to return to and recommend the healthcare provider. Thus, it was critical in those studies to identify physical environmental dimensions that affect patients’ attitudinal and behavioral outcomes. Ulrich (1984), Verderber (1986), and Wilson (1972) suggested that the existence of windows and outside views impacted patients’ experiences. Studies on the waiting area have shown the relationship between physical environmental factors and patient responses to the quality of care and approach/avoid behaviors (Arneill & Delvin, 2002; Leather, Beale, Santos, Watts, & Lee, 2003). Stern, MacRae, Gerteis, Harrison, Fowler, Edgman-Levitan, Walker, and Ruga (2003) developed an assessment tool that can explore healthcare consumers’ needs and satisfaction based on their study with a focus group that consisted of patients and family members from various healthcare facilities. The dimensions include a physical environment that “1) facilitates connection to staff, 2) is conducive to well-being, 3) is convenient and accessible, 4) is caring for family, 5) is confidential and private, 6) is considerate of impairments, 7) facilitates connection to the outside world, and 8) is safe and secure” (p. 20).
Some researchers in healthcare servicescapes have evaluated the physical environments of healthcare facilities as a whole entity, instead of separating each dimension of physical environments, to examine the impact of healthcare facilities’ physical environments on patient experiences (Becker, Sweeney, & Parsons, 2008; Delvin, 1995).
Although the number of studies on ambulatory healthcare settings is limited, there have been efforts to explore ways to improve quality of care in ambulatory healthcare. A study on wait times in outpatient facilities showed that wait time is strongly related to patient satisfaction (Leddy, Kaldenberg, & Becker, 2003). Another study developed a questionnaire to measure outpatients’ opinions on the quality of hospital consultation departments and examined evidence of a relationship between ambulatory healthcare servicescapes and perceived quality of care (Gasquet, Villeminot, Estaquio, Durieux, Ravaud, & Falissard, 2004). The questionnaire was developed to include 27 questions, of which three questions ask about servicescape dimensions such as appropriate signage, waiting room pleasantness, and cleanliness. Becker et al. (2008) showed evidence of the relationship between physical attractiveness, patient satisfaction, and perceived quality of care in their comparative study on pre- and post-moves to a new facility that was designed to be patient-centered.
Conceptual Framework
The conceptual framework for this study is premised on the notion that patients’ perceptions with servicescapes affect their satisfaction with servicescapes and perceptions with quality care, and that they will eventually lead to approach or avoidance behaviors such as willingness to recommend and willingness to return to the healthcare provider. The moderating effect of patients’ physical and emotional statuses was assumed as well in this relationship because patients’ physical and emotional statuses can lessen or intensify the impact. See Figure 1. Although Bitner (1992) suggested the conceptual framework that demonstrates the relationship between servicescapes and consumer behaviors and Hutton and Richardson (1995) further developed the framework for healthcare servicescapes, there is very scant evidence from empirical studies that tested this relationship. Newman (2007) examined the effect of spaciousness and wayfinding easiness on approach or avoidance behaviors in airport terminal shopping centers. Arneill and Delvin (2002) tested the quality of care in different waiting room designs and found that there are significant differences in perceived quality of care between waiting rooms that are warm in appearance, nicely furnished, light, and containing artwork and waiting rooms that are cold in appearance, poorly furnished, dark, and containing no artwork or low quality reproductions. Another study that examined the waiting area’s physical conditions and consumer responses compared two waiting areas before and after the relocation (Leather et al., 2003). Responses from the new waiting area indicated more positive environmental appraisals, improved moods, altered physiological states, and higher satisfaction. Design features that consumers compared included ten items such as general layout, color schemes, floor coverings, and furniture. Becker, et al.’s (2008) comparative study examined the waiting area and the exam room. Physical environmental factors compared pleasantness, privacy, and crowdedness. Responses to physical environmental factors were explored in relation to responses to quality of care, interactions with staff members, and overall experiences with the visit. Otani et al. (2010) analyzed a comprehensive patient satisfaction data set of an inpatient healthcare facility which included one attribute of a physical environmental aspect to examine its impact on perceived quality of care, willingness to recommend, and willingness to return.
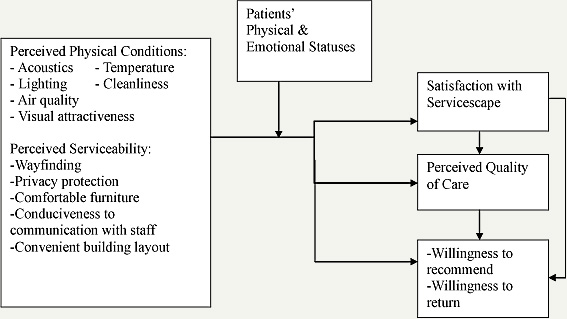
Figure 1. Conceptual framework.
This study’s conceptual framework suggests ambulatory healthcare servicescape features that affect patient satisfaction, perception, and behavior. The service design approach that focuses on patient experiences led to a list of servicescape features that include not only ambient conditions but also the serviceability of servicescapes, which may affect patients’ experiences.
Research Methods
The conceptual framework that was developed in this study is based on previous studies from various fields such as environmental psychology, marketing, and architectural design. To test the framework, a case study was conducted from the service design perspective. The study utilized the service design approach with a field survey, structured interviews, and a questionnaire survey. The study was conducted on a student healthcare clinic at an American university.
Field Survey
The student healthcare clinic is located on campus and offers various medical services. The field survey was implemented with the service design approach as in the patient journey framework (Irwin, 2002), focusing on the patient and the servicescape interactions. A patient’s possible journey was explored to understand patients’ experiences and interactions with the healthcare servicescape, evaluating whether the servicescape serves patients effectively. Service encounters with the servicescape included the exterior of the building, the reception/waiting areas, the exam area, and exiting of the facility. Photographs were taken for the analysis of space layout and physical traces and the identification of design issues. The patient-centered servicescape criteria were developed for this field survey based on and modified from the patient-centered environmental checklist (Stern et al., 2003). The criteria of this study included ambient conditions such as lighting, noise, temperature, communication with staff, accessibility/wayfinding, privacy, and safety/security. The field survey was used to identify problems and issues of service encounters, and the structured interview tool was developed based on results from the field survey.
Structured Interviews
The convenience sampling method was used to recruit participants for the survey. There were 22 students who participated in the interview, consisting of 15 females and 7 males. The first section of the interview tool included questions about demographic information and physical/emotional statuses. The second section included questions about transportation methods and the number of previous visits. The third section included questions about the serviceability of the servicescape, e.g., outdoor wayfinding, indoor wayfinding, visual quality, waiting room design, exam room design, daylighting, and cleanliness. The fourth section included questions about the quality of care and willingness to return. The results from the structured interviews were used in the development of the questionnaire tool for this study.
Questionnaire Survey
There were 170 students who participated in the survey. The students that had already visited the facility were invited to participate in the survey, and 151 completed survey data sets have been analyzed for the study. The survey tool was composed of 42 questions. In the questionnaire, section 1 included background information questions about age, gender, and number of previous visits. Section 2 included questions about wayfinding such as easiness of entrance finding, the reception area, the check-in, the check-out, and the restroom. One question asked if the signage helped in wayfinding. Section 3’s questions asked about the physical and emotional statuses of patients, such as distress, feelings of physical weakness, and discomfort. Section 4 was comprised of a set of questions about the reception and waiting areas. Questions asked if privacy was respected while talking to staff members, if it was easy to hear or see staff members when they called patients, if the number of seats was adequate in the waiting area, if it was noisy, if seating was comfortable, if lighting was adequate, and if the layout of the waiting area was convenient. Section 5 had questions about the clinical area concerning the comfort of furniture, comfort of lighting, comfort of temperature, visual attractiveness, and privacy. Section 6’s questions evaluated patients’ perceptions with the overall facility with questions about ambient conditions such as temperature and lighting and about serviceability such as the respect of privacy and convenience of layout. Section 7 consisted of questions about patients’ satisfaction with the facility such as cleanliness, visual attractiveness, ambient conditions, and wayfinding. Section 8’s questions inquired about the perceived quality of care, willingness to recommend the facility, willingness to return to the facility, and willingness to go to another facility if they had the option. Sections 2-7 were measured using a 5-point Likert scale (1=strongly disagree; 5=strongly agree).
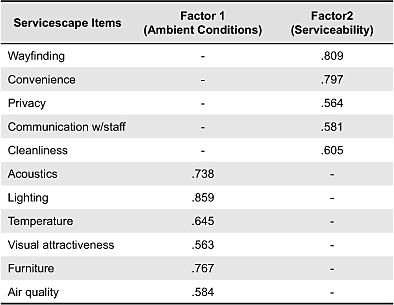
The following statistical analyses were undertaken to study the survey data. All analyses were conducted using SPSS 18 for Windows. First, principal components factor analyses with Varimax rotation with Kaizer normalization for the items in the servicescape scale were conducted to assess whether the items factored into the following two constructs: ambient conditions and serviceability. Examination of Eigenvalues, scree lot, and factor loadings all indicated a two-factor solution: ambient conditions and serviceability. See Table 1 for factor loadings. Next, zero-order correlation analyses were employed to determine the bivariate relationships between the independent variables and the dependent variables. After the correlations were explored, multiple regression analyses were used to examine (1) the contributions of the sets of predictor variables in explaining the variance in the criterion variables, and (2) the significance level of specific beta coefficients within the models (Pedhazur, 1982). As a precaution against multicollinearity, tolerance tests were conducted using the default value of .10 as the low level for tolerance (Cohen & Cohen, 1983). The conceptual framework has been tested with correlations and regression analyses. In regression analyses, the relationships between perceptions with servicescapes and satisfaction with the facility were tested. After the regression model of satisfaction with the facility was tested, the relationships between perceptions with servicescapes and perceptions with quality of care were tested. The relationships between perceptions with servicescapes and willingness to return and recommend were tested next. The moderating effect of physical and emotional statuses on the relationship between perceptions with servicescapes and three dependent variables was not tested. Although the moderating effect was assumed in the conceptual framework, it did not show any causal relationship with any of the dependent variables.
Table 1. Structure matrix loadings.
Results
Field Survey
The field survey was conducted based on patient-centered servicescape criteria following a patient’s possible journey in the facility. The criteria included ambient conditions such as lighting, noise, temperature, communication with staff, accessibility/wayfinding, visual aspects, and privacy.
Exterior of the Building
The exterior of the building has similar architectural features as the rest of the buildings on campus. There are two entrances to the building: the front door and the back door. The front door is near the sidewalk. The back door is next to the parking lot connected to the street. There is no sign on the front of the building except one on the glass door at the entrance. On the back side of the building, there is a low and small sign pointing to urgent care. With minimal signs outside, it is hard to find the building if the visitor does not know that the building is the student health clinic. There are seven parking spots available for students that are fully occupied during most of the office hours.
Reception/Waiting Areas
The patient reception area is located by the front entrance when one immediately walks in the facility. The reception area is open to the waiting area and connects to the business offices. During busy hours in the day, lines of patients form and become an obstruction for the path of passing traffic between the waiting area and business offices. There are signs located on the counters to designate the check-in and check-out counters, but it is difficult to see those signs when lines of patients begin to form.
The waiting area is a long hallway connecting the two entrances, surrounded by the physicians’ offices. Since the waiting area is an open corridor and serves as the main means of egress, waiting patients are exposed to the path of traffic continually passing by. The long corridor and abundance of doors may cause confusion as to where the patient will be called. The noise level is dominantly low with the exception of busy times during the cold season, when individuals have cold symptoms such as sniffing and coughing. The lighting in the waiting area is all-fluorescent with no natural light. In addition, the dark and outdated finishes in the area create a cave-like atmosphere. The selection of furniture is predominantly chairs that limit patients from lying down to become fully comfortable. The orientation of the pieces of furniture facing each other may cause patients to feel uncomfortable when facing each other.
Clinical Area
The exam area is connected to the waiting area and the nurses’ room next door. The exam room is plain with white walls and plain cabinets, creating a clean but stark atmosphere. A large window in each exam area creates abundant natural light for the patient. The exam room also serves as the physician’s personal office.
Overall Facility and Exiting
The facility’s temperature and noise level seem to be at a comfortable level. The facility has daylighting in the clinical area, but the waiting area did not have access to daylighting. The facility was clean but had an outdated look due to the finishes and materials. Exiting the building can be confusing due to the existence of two exits. Also, once a patient leaves the exam room, he/she enters a large corridor with no structural or signage indication as to where he/she should be directed.
Structured Interviews
The structured interviews yielded findings that revealed patient experiences with the servicescape and served as guides to develop questions for the questionnaire tool. The same criteria from the field survey were used to report findings from the structured interviews.
Exterior of the Building and the Reception Area
Participants in this study were university students, and most of them were already aware of the facility’s location from the campus map or from passing by the facility previously. Most participants walked to the facility. Participants who drove to the facility found parking difficult. From the outside of the building, they reported wayfinding issues. When it was hard to find the emergency door, the patients were especially frustrated. In the building, patients needed to find the reception area to check in. Participants reported that this was also hard to find unless a line had already formed.
Reception/Waiting Areas
Due to the layout of the waiting area, participants reported discomfort. The waiting area is located in the middle of the building, and doctors’ offices are laid out around it. In addition, there are exits on both ends of the waiting and clinical areas. When participants enter the building from the back door, they need to pass through the waiting area. People who sit in the waiting area felt that they were in the middle of the hallway and were therefore too exposed. Patients needed to pay attention to hear or see staff calling them because they were not sure where and when they would be called in.
Participants reported that they felt that they were surrounded by too many sick people. There were no complaints about the temperature or lighting, but many reported unwanted sounds and noises such as other patients coughing, the TV, and doctors’ conversations with other patients that they did not want to hear. Participants who were in pain wanted to lean back in the waiting area, but the seating did not support leaning back.
Patients mentioned that the waiting area is not visually pleasing and wanted the area to be more cheerful and relaxing. They suggested more comfortable seating for sick people and a less boring and dull environment. One positive aspect of the waiting area was that there were resources to read while the patients were waiting.
Clinical Area
In the clinical area, participants reported some discomfort with lighting, temperature, noise, and medical supplies in the cabinet being exposed. The main complaint about the lighting was that the fluorescent lighting was too bright and gave an institutional feeling that brought about negative feelings. Participants who complained about the temperature felt that it was too low; no one complained about it being too high. The exam area in the emergency room was too exposed to other patients, and participants didn’t want to hear or see other patients. Medical supplies in the exam area were labeled, exposed visually, and were not securely stored in cabinets for patients. This made participants feel intimidated.
Pictures or decorative elements such as posters made participants feel more comfortable. In the exam room, the only seating that was available for patients was the exam table. Participants wanted to have an extra chair to sit on instead of sitting on the exam table while they were waiting for the doctor. Participants also reported that the exam room was cluttered with medical instruments. Participants who used the services in the basement reported that the room was too dreary. Although exam rooms on the first floor had daylighting, participants were bothered when they did not like the view, such as fraternity party scenes, as one participant mentioned.
Exiting
Participants experienced less trouble finding their way out than in. However, finding their way out was still not easy for first time visitors or those who had to find their way out from the basement.
Questionnaire Survey
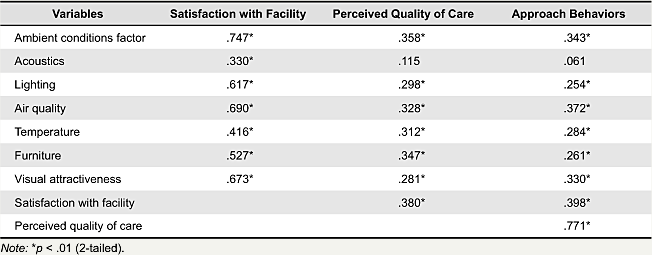
Two correlational analyses have been conducted in this study. The first correlational analysis included individual variables, perceived wayfinding, perceptions with each area, satisfaction with the facility, perceived quality of care, and approach behavior. See Tables 2 and 3. The second correlational analysis included individual, ambient condition, and serviceability variables. The area variables in the first correlational analysis were categorized by each area, such as the reception/waiting areas, the clinical area, and the overall facility, while the second analysis categorized the predictor variables into ambient condition variables and serviceability variables to test the conceptual framework. Based on the factor analyses that have been conducted in this study, ambient conditions factor included acoustics, lighting, air quality, temperature, furniture, and visual attractiveness. Serviceability factor included variables that facilitate patients’ activities such as wayfinding, convenient facility design, privacy, communication with staff, and cleanliness.
Participants who were younger perceived wayfinding more easily. There were no significant relations between age and perceptions with servicescapes other than wayfinding. The physical status of participants, including sickness and emotional distress, showed significant relations with perceptions with the waiting area’s servicescape and perceptions with the overall facility’s servicescape. See Table 2.
Table 2. Correlations between individual variables and perceptions.
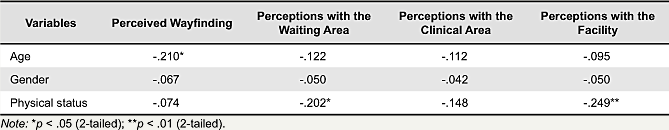
When participants were more sick and emotionally distressed, they were less satisfied with the physical conditions of the facility. Participants also showed lower perceived quality of care and less willingness to come back or recommend the healthcare to others. See Table 3. Perceptions with each area’s servicescape features showed significant relations with satisfaction with the facility, perceived quality of care, and willingness to return and recommend. The relationship tends to be stronger for perception with the overall facility rather than for each individual area. See Table 3.
Table 3. Correlations of satisfaction, perceptions, and behaviors.
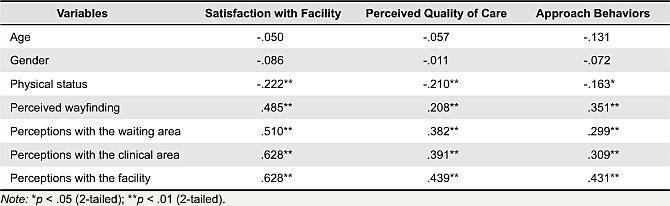
The next set of correlational analyses have been conducted to assess correlations between dependent variables and servicescape variables that include ambient conditions factor and serviceability factor. See Tables 4 and 5. Overall, serviceability factor showed stronger relations to dependent variables.
In correlations of ambient conditions factor and dependent variables, perceptions with acoustics showed relations with satisfaction with facility. However, no significant relations were detected with perceived quality of care and approach behaviors, such as willingness to return and recommend. Perceptions with air quality and furniture showed stronger relations with perceived quality of care compared to other ambient conditions factor. In relationships with approach behaviors such as willingness to return, recommend, or go to other healthcare when there is an option, perceptions with air quality and visual attractiveness showed the strongest relations. See Table 4.
Table 4. Correlations between ambient conditions factor and satisfactions, perceptions, and behaviors.
The serviceability factor showed stronger relations with satisfaction with facility, perceived quality of care, and approach behaviors compared to ambient conditions factor. Convenient design and cleanliness were two variables that showed stronger relations to satisfaction with facility. Wayfinding and cleanliness were the two strongest variables in relation to perceived quality of care. In relation to approach behaviors, serviceability factor showed similar strength in their relations, and the order, from strongest to weakest, was cleanliness, convenient design, perceived wayfinding, communication with staff, and privacy.
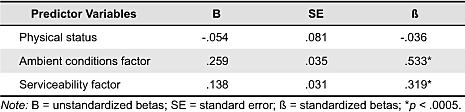
Multiple Regression Analyses
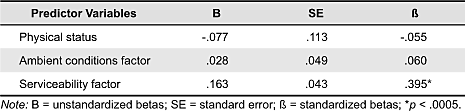
The first multiple regression analysis has been conducted to examine the relationship between satisfaction with facility and predictor variables such as physical status, ambient conditions factor, and serviceability factor. Using the enter method, a significant model emerged: F (3,131) = 73.157, p < .0005. The model explains 61.8% of the variance (adjusted R2 = .618). Table 6 shows information for the predictor variables entered into the model. The findings suggest that ambient conditions factor and serviceability factor were significant predictors of satisfaction with facility. Although the physical status of patients showed correlations with satisfaction with facility, it did not show any causality in the multiple regression model.
Table 5. Correlations between serviceability factor and satisfactions, perceptions, and behaviors.
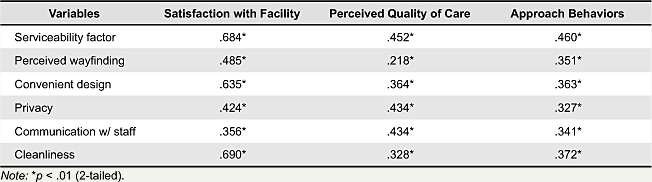
Table 6. Multiple regression model: Satisfaction with facility.
The second multiple regression analysis was to examine the relationship between perceived quality of care and physical status, ambient conditions factor, and serviceability factor. The same set of predictor variables that were used in the multiple regression model of satisfaction with facility was entered into this analysis model. The model showed a significance of p < .0005 with F (3,131) = 11.471. The model explains 19% of the variance (adjusted R2 = .190). The physical status and ambient conditions factor were not significant predictors, but the serviceability factor was. Although this model explains only 19% of the variance of perceived quality of care, it still shows great significance. It is important to note that the serviceability of the healthcare servicescape serves as a significant predictor of patients’ perceived quality of care while ambient conditions factor does not.
The third model of regression analysis also used the enter method. The model was statistically significant: F (3,131) = 11.100, p < .0005. The model explains 18.4% of the variance (adjusted R2 = .184). Table 8 gives information for the predictor variables entered into the model. Similar to the regression analysis model with perceived quality of care, serviceability factor was the only variable that predicted approach behavior factors such as willingness to return, willingness to recommend, and willingness to go to other healthcare when patients have the option (reversely coded) in this regression analysis model. This indicates that when patients feel that wayfinding is hard in the facility, their privacy is less protected, the furniture is less comfortable, communication with the staff is hard, and the design of the facility is not convenient for their activities in the facility, they may not be willing to return to the facility or recommend it to other people, and will instead want to go to other healthcare when they can.
Table 7. Multiples regression model: Perceived quality of care.
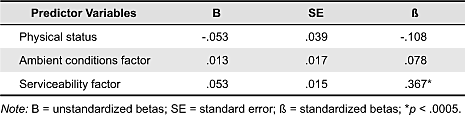
Table 8. Multiple regression model: Approach behavior.
Discussion
Results from the field survey have revealed that wayfinding in this facility was not easy for patients, especially for first time visitors who were not familiar with the facility. In addition, the layout of the waiting area seemed to create an inconvenient and uncomfortable environment for the purpose of waiting because it was located in the middle of two entrances. Results from structured interviews supported the findings from the field survey. Participants reported that wayfinding was not easy to access the facility and find ways inside of the building. The waiting area’s layout was mentioned by participants as uncomfortable because they felt they were too exposed to the traffic between the back entrance and the reception area. The layout of chairs in the waiting area made participants uneasy because they were forced to face each other. Participants also reported that communication with staff such as the staff members calling them in to the clinical area was not convenient due to the layout of the waiting area design. It was hard for patients to see where the staff would come out to call them. This result supports a previous study (Stern et al., 2003) in that patients and family members want healthcare facilities to facilitate communication with staff.
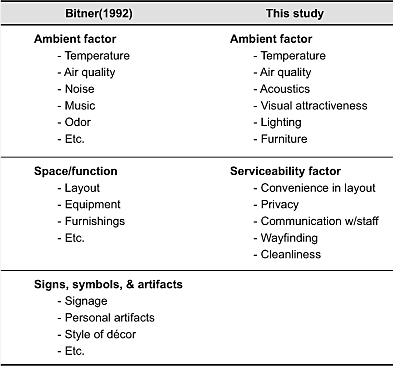
The conceptual framework that was developed earlier in this study was tested with statistical analyses. The conceptual framework was based on Bitner (1992) and Hutton and Richardson (1995). However, there is a difference in servicescape dimensions between those studies and this study. This study assumed two factors as servicescape dimensions, ambient conditions and serviceability, while Bitner (1992) and Hutton and Richardson (1995) assumed three factors as servicescape dimensions, ambient conditions, space/function, and signs/symbols/artifacts. This study integrated the space/function factor and the signs/symbols/artifacts factor into one because signs and symbols relate to wayfinding, which serves patients’ activities just as space and function do. Factor analyses showed that there are two components of servicescape features, as this study assumed. The ambient conditions factor included acoustics, lighting, air quality, temperature, furniture, and visual attractiveness. The serviceability factor included wayfinding, convenient design, privacy, communication with staff, and cleanliness. This result indicates that patients perceive serviceability items as features that serve their activities and facilitate their purposes in the facility.
Most servicescape items showed correlational relations with satisfaction with facility, perceived quality of care, and approach behaviors. This means that when patients’ perceptions with physical conditions and serviceability of ambulatory healthcare are higher, they feel more satisfied with the facility, perceive quality of care more highly, and are more willing to return to and recommend the healthcare. These effects of servicescape on patient perceptions with satisfaction, quality of care, and approach behaviors have been suggested in previous studies (Arneill & Delvin, 2002; Leather et al., 2003; Newman, 2007; Otani et al., 2000) and this study supports the evidence.
Physical status was also assumed to affect patients’ experiences. Although it showed negative correlations with satisfaction and approach behaviors, it did not appear to cause those experiences. Therefore, the moderating effect of physical status from patients’ perceptions with servicescapes to patient experiences was not explored in this study. Results indicate that perceptions with facility lead to satisfaction with facility as both ambient conditions factor and serviceability factor affected patients’ satisfaction with facility. In addition, findings from this study suggest that serviceability factors are more significant and powerful to influence patients’ perceptions with quality of care and willingness to return to and recommend the healthcare provider compared to ambient condition factors. Thus, this study suggests for future studies in ambulatory facility servicescapes to include serviceability items such as cleanliness of servicescape, convenient wayfinding, convenient layout design, and facilitations to communication with staff and protection of privacy. Although there are studies that examined one or two serviceability factors such as wayfinding (Newman, 2007), cleanliness (Otani et al., 2000), and layout (Leather et al., 2003), it will be important to approach patients’ perceptions with servicescapes more holistically, as it is practiced in service design research.
Conclusion
This study aimed to examine ambulatory healthcare servicescapes from a service design approach using a design methodology that focused on users and their interactions with the built environment. It implemented a research methodology that explored patients’ experiences in ambulatory healthcare facilities. First, a conceptual framework was developed based on previous studies. A field survey, structured interviews, a questionnaire survey, and analyses were conducted to test the conceptual framework. The questionnaire tool was developed based on the findings from the field survey and the structured interviews.
Several findings were evidenced through this investigation. First, factor analyses revealed that there are two dimensions in servicescape features including ambient conditions factor and serviceability factor. This result is different from those studies (Bitner, 1992; Hutton & Richardson, 1995) that suggested servicescape dimensions as three factors: ambient conditions, space/function, and signs/symbols/artifacts. See Table 9 to compare servicescape factors between Bitner’s (1992) and this study’s. As the table shows aspects of ambient factor are similar across two studies. Bitner (1992) separated signs, symbols, and artifacts as an aesthetic factor that provides the first impression. However, this study recognized the value of signs and symbols that serve wayfinding and included wayfinding as an aspect of serviceability factor. Considering that this study is based on an empirical research method, it is suggested that future studies examine this issue further.
Table 9. Servicescape factors.
Secondly, physical status was detected to be correlated with satisfaction with facility, perceived quality of care, and approach behaviors. However, it does not appear to be a predictor of these variables. Thirdly, serviceability factor was the more significant and powerful type of factor to impact patients’ perceived quality of care and approach behaviors compared to ambient conditions factor. The serviceability factor includes aspects that relate to the quality of the environment that serves building users such as wayfinding, convenience, privacy, communication with staff, and cleanliness.
This study provides important insights for ambulatory healthcare facility designers and providers. Ambulatory healthcare servicescapes can be approached from a service design perspective to create patient-centered healthcare.
References
- Arneill, A., & Delvin, A. (2002). Perceived quality of care: The influence of the waiting room environment. Journal of Environmental Psychology, 22(4), 345-360.
- Becker, F., Sweeney, B., & Parsons, K. (2008). Ambulatory facility design and patients’ perceptions of healthcare quality. Health Environments Research and Design Journal, 1(4), 35-54.
- Bitner, M. (1992). Servicescape: The impact of physical surroundings on customers and employees. Journal of Marketing. 56(2), 57- 71.
- Brown, T. (2008). Design thinking. Harvard Business Review, 86(6), 84-92.
- Bureau of Labor Statistics, U.S. Department of Labor. (2010). Career guide to industries, 2010-11 edition. Retrieved August 23, 2010, from http://www.bls.gov/oco/cg/cgs035.htm
- Carpman, J., & Grant, M. (1993). Design that cares: Planning health facilities for patients and visitors (2nd ed.). San Francisco: Jossey-Bass.
- Cohen, J., & Cohen P. (1983). Applied multiple regression analysis for the behavioral sciences (2nd ed.). Hillsdale, NY: Erlbaum.
- Fottler, M., Ford, R., Roberts, V., & Ford, E. (2000). Creating a healing environment: The importance of the service setting in the new consumer-oriented healthcare system. Journal of Healthcare Management, 45(2), 91-106.
- Francis, S. (2010). Plan for uncertainty: Design for change. In M. Kaioglou & P. Tzortzouplos (Eds.), Improving healthcare through built environment infrastructure (pp. 4-52). Oxford: Blackwell.
- Gasquet, I., Villeminot, S., Estaquio, C., Durieux, P., Ravaud, P., & Falissard, B. (2004). Construction of a questionnaire measuring outpatients’ opinion of quality of hospital consultation departments. Health and Quality of Life Outcomes, 2(1), 43.
- Hutton, J., & Richardson, L. (1995). Healthscapes: The roles of the facility and physical environment on consumer attitudes, satisfaction, quality assessments, and behaviors. Health Care Management Review, 20(2), 48-61.
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC: The National Academy of Sciences.
- International Code Council. (2009). 2009 international building code. Washington, DC: International Code Council.
- Irwin, R. (2002). IDEO’s design cure. Metropolis. Retrieved July 15, 2010, from http://www.ideo.com/images/uploads/thinking/publications/pdfs/metropolis_1.pdf
- Kotler, P. (1973). Atmospherics as a marketing tool. Journal of Retailing, 49(4), 48-64.
- Leather P., Beale D., Santos A., Watts J., & Lee L. (2003). Outcomes of environmental appraisal of different hospital waiting areas. Environment and Behavior, 35(6), 842-869.
- Leddy, K., Kaldenberg, D., & Becker, B. (2003). Timeliness in ambulatory care treatment. An examination of patient satisfaction and wait times in medical practices and outpatient test and treatment facilities. Journal of Ambulatory Care Management, 26(2), 138-149.
- Lin, B., Leu, W., Breen, G., & Lin, W. (2008). Servicescape: Physical environment of hospital pharmacies and hospital pharmacists’ work outcomes. Health Care Management Review, 33(2), 156-168.
- Maffei, S., Mager, B., & Sangiorgi, D. (2005). Innovation through service design. From Research and theory to a network of practice. A users’ driven perspective. Retried July 12, 2010, from http://www.service-design-network.org/system/files/10_Mager_Innovation_0.pdf
- Martin, R. L. (2009). The design of business: Why design thinking is the next competitive advantage. Boston: Harvard Business Press.
- Moritz, S. (2005). Service design: Practical access to an evolving field. Cologne: Koln International School of Design.
- Newman, A. (2007). Uncovering dimensionality in the servicescape: Towards legibility. The Service Industries Journal, 27(1), 15-28.
- Otani, K., Waterman, B., Faulkner, K., Boslaugh, S., & Dunagan, C. (2010). How patient reactions to hospital care attributes affect the evaluation of overall quality of care, willingness to recommend, and willingness to return. Journal of Healthcare Management, 55(1), 25-37.
- Parasuraman, A., Zeithaml, V., & Berry, L. (1988). SERVQUAL; A multiple-item scale for measuring consumer perceptions of service quality. Journal of Retailing, 64(1), 12-40.
- Pedhazur, E. J. (1982). Multiple regression in behavioral research and prediction. New York: Hartcourt Brace College Publishers.
- Rubin, H. (1997). The relationship between environmental design and patient medical outcomes. Journal of Healthcare Design, 9, 13-14.
- Stern, A., MacRae, S., Gerteris, M., Edgman-Levitan, S., Walker, J., & Ruga, W. (2003). Understanding the consumer perspective to improve design quality. Journal of Architectural and Planning Research, 20(1), 16-28.
- Ulrech, R. (1984). View through a window may influence recovery from surgery. Science, 224(4647), 420-421.
- Verderber, S. (1986). Dimensions of person-window transactions in the hospital environment. Environment and Behavior, 18(4), 450-466.
- Verderber, S., & Fine, D. (2000). Healthcare architecture in an era of radical transformation. New Haven, CT: Yale University Press.

