Design Concepts for Digital Diabetes Practice: Design to Explore, Share, and Camouflage Chronic Illness
Anne Marie Kanstrup
Department of Communication, Aalborg University, Aalborg, Denmark
This paper examines design of digital support for people living with chronic diabetes. It identifies three design concepts for digital diabetes practice. These were developed during a four-year research project investigating everyday life activities related to diabetes. Social learning theory frames the conceptualisation of how to understand and design for diabetes practice. The focus on the practice of chronic illness addresses the need to re-think digital health technology and expands possible solutions beyond the medical condition itself. The study shows the importance of attention to everyday practice and contributes a conceptual understanding of the tensions between medical ideals and the everyday lives of people with chronic illness.
Keywords – Design Concepts, Digital Health Services, Diabetes, Participatory Design, Social Learning Theory.
Relevance to Design Practice – The conceptualisation of digital diabetes practice can prepare designers for action within the medical engineering landscape of digital support for diabetes and related chronic illnesses.
Citation: Kanstrup, A. M. (2014). Design concepts for digital diabetes practice: Design to explore, share, and camouflage chronic illness. International Journal of Design, 8(3), 49-60.
Received June 7, 2013; Accepted June 1, 2014; Published December 31, 2014.
Copyright: © 2014 Kanstrup. Copyright for this article is retained by the author, with first publication rights granted to the International Journal of Design. All journal content, except where otherwise noted, is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 2.5 License. By virtue of their appearance in this open-access journal, articles are free to use, with proper attribution, in educational and other non-commercial settings.
Corresponding Author: kanstrup@hum.aau.dk.
Anne Marie Kanstrup is a Professor in Human Centered Informatics at the Department of Communication, Aalborg University. Her research focuses on the development of theories and methods for the participatory design of information systems. Kanstrup’s primary research area is Health Informatics with a research focus on the design of information systems that support patients and health care professionals in their everyday living and working with health. Her research includes a series of projects within the areas of chronic illness, health promotion and computerized physician order entry, studies of patient innovations and methods and tool-kits for user innovation management.
Introduction
The paper examines digital design to support daily living with the chronic illness of diabetes. The design ambition of the study is rooted in Papanek’s (1984) definition of design responsibility as engagement with “real problems”. This includes a broad perspective on human ecology. Papanek illustrated this with a triangle (Figure 1), which depicted designers as working only in the top segment, thus exhibiting a “lack of social engagement in design” and being responsible for bad design due to “not getting involved” (Papanek, 1984, p. 56). Designing for the real world calls for engaging with peoples’ real problems, that is, the lower part of Figure 1. Recent literature on design and medicine calls attention to this need to engage with people’s real problems and practices in contrast to a focus solely on a given medical condition. One example of this is Pullin’s (2009) analysis of a series of products designed to support people with disabilities. Pullin shows how design can contribute to broadening the traditional medical engineering perspective on illness and the body by engaging with people’s everyday lives and including qualities related to everyday practice, emotions, identity, etc. in the product design. Even in hospital settings, there are calls for “thinking beyond the cure” and expanding the solution space of medical technology to include patients’ emotional well-being (Mullaney, Pettersen, Nyholm, & Stolterman, 2012). This paper supports these calls for design grounded in engagement with peoples’ everyday practices. It presents results from a long-term participatory design research project in which the objective was to design digital support for everyday living with diabetes in co-operation with 17 families affected by the illness.
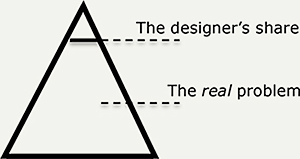
Figure 1. Papanek’s (1984) visualisation of designer’s responsibility to focus on problems of everyday life.
Diabetes is a serious chronic illness, especially type 1 diabetes, which requires strict control of the blood glucose level. This is obtained by balancing a triangle of food, exercise and insulin (Figure 2).
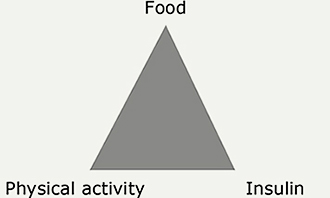
Figure 2. The clinical model of diabetes management.
Diabetics must measure their blood glucose level several times a day and calculate carbohydrate intake, insulin dosage and physical activity. These activities are termed “self-management”. If the diabetic fails to self-manage (forgets to monitor, miscalculates, is ill from influenza, etc.) the consequences can be severe. Short-term imbalances in the triangle of diabetes (Figure 2) are called hypoglycaemic episodes. They cause various physical and psychic symptoms and may lead to unconsciousness. Manifest hyperglycaemia can lead to an internal poisoning-like condition known as a diabetic coma, which can lead to death. Chronic moderate hyperglycaemia implies an increased risk for early and severe late-stage diabetes complications.
Digital technology designed to support diabetics is primarily anchored in the clinical perspective of individual self-management (Figure 2), just as most self-management programs deal only with medical management (Lorig & Holman, 2003, pp. 2-3). Typical self-management technologies for diabetes are software applications into which diabetics enter their blood glucose measurements, insulin doses and food intake, monitor changes in glucose level and learn from this (Boisen, Bygholm, Cavan, & Hejlesen, 2003). This primary focus on illness and the body, in contrast to engagement with people and practices, can be interpreted as either underestimating the importance of everyday practices in the management of chronic illness or representing the difficulty of designing for this expanded solution space.
The research question this paper addresses is how to expand digital design for diabetes to encompass attention to daily life with a chronic illness. This question has guided research on everyday life activities related to diabetes and the exploration of digital designs for these activities. The paper presents an analysis of research results where everyday life activities and core tensions related to diabetes practice are identified. On this basis, three design concepts for digital diabetes practice are developed. The conceptualisation of everyday diabetes practice and the related design concepts constitute answers to the research question. Firstly, the paper shows why everyday practice is important to the design of digital support for diabetes. This is accomplished using references to the literature and empirical data from a four-year participatory design research project that sought to design digital support for everyday living with diabetes. The study shows why attention to everyday practice when designing digital support for chronic illnesses is important. It contributes a conceptual understanding of the tensions between medical ideals and people’s everyday lives. Secondly, it introduces social learning theory as a framework for understanding practice. This framework is applied to results obtained by exploring digital prototypes within the research project. From this analysis, the three design concepts emerge. These are design to explore, design to share and design to camouflage chronic illness. The temporal and spatial aspects of the identified design concepts are discussed, contributing to conclusions regarding the concepts’ value for digital design supporting diabetes and chronic illness in general.
Chronic Illness in Everyday Practice
Sociological studies provide nuanced understandings of activities related to everyday life with chronic illness. Corbin and Strauss’s (1988) qualitative study is extensively cited and delineates the three main tasks faced by people living with chronic illness. The first set of tasks involves medical management, such as taking prescribed medicine, monitoring blood glucose levels, following a given diet, etc. The second set of tasks relates to maintaining and creating meaningful behaviours and life roles at work, with family and friends, and during leisure time. For example, illness can force adjustments in work tasks, participation in sport activities or housework. The third set of tasks involves dealing with emotions related to living with chronic illnesses. People with chronic illnesses commonly experience emotions such as anger, fear and depression (Corbin & Strauss, 1988). Reviews of self-management emphasise the importance of people’s feelings of self-efficacy (Lorig & Holman, 2003). People’s ability to deal with the complexity of everyday life with chronic illness is fundamental because “self-efficacy represents a generative capability in which multiple subskills must be flexibly orchestrated in dealing with continuously changing realities, often containing ambiguous, unpredictable, and stressful elements” (Bandura, 1984, p. 233). These research results emphasise the comprehensiveness of the practice of living with chronic illness—people’s ability to master multiple skills, flexibility, emotions, ambiguity, unpredictability and the creation of meaning in everyday life with chronic illness.
Literature focused on the design of digital technology for everyday life with chronic illness calls attention to the gap between the above understandings of everyday practice and technologies that are designed solely to support the self-management of the medical condition. The main critiques of the majority of technologies designed to support the monitoring of blood glucose levels for example are that they miss the opportunity to support the “boundary work” between illness and everyday life (Aarhus & Ballegaard, 2010), that is, the connections between the illness and the “multiple subskills” used to create and maintain meaningful behaviours and emotions related to everyday life with a chronic illness. Additionally, there is a critique of the conceptual model of traditional technologies for diabetes self-management because they “rely on a naïve assumption that once the data is collected and presented to the individuals, they will draw appropriate inferences unproblematically” (Mamykina, Mynatt, & Kaufman, 2006, p. 927). The conceptual model found in most diabetes self-management technologies regards the illness as “a given object to be managed” and misses the point that diabetes is “a practiced object” (Danholt, 2008, p. 15). This supports the call for expanding the solution space beyond the medical condition via design (Mullaney et al., 2012; Pullin, 2009).
Everyday Diabetes Practice in the Design Case
The point of departure for the design case reported is to go beyond the majority of digital designs for diabetes, which focus primarily on the self-management of the medical condition and move towards design for everyday life with diabetes by including equally important subtasks related to people’s lives with chronic illness (Bandura, 1997; Corbin & Strauss, 1988). The research question of how to expand the solution space of digital design for chronic illness was fundamental to the design case. The approach used to answer this question was to engage in people’s everyday lives with diabetes (Papanek, 1984) through participatory design (Greenbaum & Kyng, 1991; Robertson & Simonsen, 2012). As with related design research, the approach sought to explore how the participation of people affected by illness can contribute to expanding the solution space surrounding the medical condition (Mullaney et al., 2012). This involved relying on empathy with the user group rather than existing standards and guidelines (Newell, Gregor, Morgan, Pullin, & Macaulay, 2011). The design case included a series of participatory design methods with the objective of understanding and transcending digital diabetes practice.
Methods
Between 2007 and 2011, 17 families from Northern Denmark (60 people in total) with one or more diabetic members participated in the research project, “the maXi-project”, an acronym for mastering chronic illness with Information and Communication Technology. The design process included two major iterations. Eight families participated in the first iteration. Nine families participated in the second iteration. Participants were selected to represent a broad variety of the target group, being aged from four to 68 years old. Approximately 50% were type 1 diabetics and approximately 50% were type 2 diabetics. Some were newly diagnosed. Others had more than 20 years of experience living with diabetes. The families were distributed over a large area of Northern Denmark. Some lived in the country and others lived in small or medium-sized cities. Although the participants varied in several ways, they were a relatively homogeneous social group of middle-class Danish families.
The project was rooted in participatory design research to explore how people affected by diabetes can contribute to expanding the solution space of digital diabetes technology. A variety of participatory design methods were used (Greenbaum & Kyng, 1991; Kanstrup & Bertelsen, 2011). In total, all families participated in 1) two hours of home interviews followed by one week of postcard writing, 2) three-hour workshops at the university, and 3) one weekend of exploring prototypes for digital health services in a living laboratory, a semi-naturalistic technological set-up of digital services in co-operation with service providers in the city of Skagen. This concluded with a design workshop. The families participated in their spare time. Effort was made to make participation appealing and practicable by limiting activities to two hours in duration, performing at-home interviews and workshops, and locating the living lab experiments within the city of Skagen, a popular vacation site due to its beautiful scenery and culture.
During the home interviews, visual tangible artifacts in the form of laminated photographs of places (streets, sport centres, nature, homes, cinemas, schools, workplaces, etc.) were developed to support the participation of all family members and to make the subject of the conversation concrete. The family members and researchers gathered around the family’s dinner table. Each family member was asked to select three photo-cards representing places where they needed support related to diabetes. In turn, the family members disclosed which photo-cards they had taken and explained why they had done so. In this way, turn taking was ensured. All family members could participate, even toddlers, and the participants were pushed to reflect on their daily activities and needs related to diabetes. After the photo-card interview, all family members were given seven postcards, one for each day of the week, with the pre-written question: “Where are you, and what would you like to know?” The postcards were intended to continue the data collection after the interview based on real-time situations. The families returned 72 postcards. Teenagers and introverted participants, who had been rather short on words during the home-interviews, were especially active in writing postcards, stressing the importance of using complementary methods of participation. Each home-interview ended with a photo of the collection of materials the family currently uses for support during their day-to-day lives with diabetes.
At a workshop, the families and researchers co-operated on the analysis of problems identified during the interviews and postcard writing. One part of the workshop focused on problems related to grocery shopping, especially problems related to reading and understanding lists of food contents. One part of the workshop focused on problems experienced by diabetics at restaurants, bakeries and venues where food does not have labelling. One part of the workshop focused on learning about diabetes. The last part of the workshop focused on collaboration within the family. During each workshop-part, the primary findings from the interviews and postcard writings were presented, along with an exercise asking participants to prioritize, supported by Venn diagrams (Mukherjee, 2002); create alternatives, supported by sketching (Buxton, 2010); and debate problems, supported by design games (Brandt, 2006; Brandt, Messeter, & Binder, 2008).
Diabetes Practice
The comprehensiveness of diabetes practice was clear from the beginning. When participants were asked to share their core situations and needs regarding digital support, a broad pattern of activities related to diabetes surfaced (Kanstrup, Bertelsen, Glasemann, & Boye, 2008). The calculation central to the diabetes triangle (Figure 2) was presented by all participants as an ongoing key activity that formed a part of every other related activity. Examples were as follows: “It is difficult to be in restaurants because you cannot count anything. How many vegetables are there, how much fat is there, can we avoid the sauce, and when will the food arrive?” (partner of diabetic). “Exercise is very difficult. In the morning, it is difficult to know how much she will exercise during they day. If it is raining, I will imagine that she will stay in-doors and have a quiet day. If the sun is shining, I will imagine that she will be out playing most of the time” (parent of diabetic child). “I always check sodas with my blood glucose meter, and often, it is not the diet soda that I ordered, and then, I get an apology and another soda” (diabetic adolescent). Calculation is especially important in handling unknown quantities and, as a consequence, in managing uncertainty, making informed guesses, maintaining control and building up experience. This is not supported by existing technologies. Consequently, diabetics carry out these tasks by estimating, taking chances or avoiding difficult situations. In general, the calculations are not merely arithmetic and cannot be based on the measurement of blood glucose levels alone. A set of related core activities were described by the participants, including co-operation. For example, family members co-operate regarding calculations, “tricks of the trade”, inspiration and experiences: “I call my parents during the breaks at school and tell them that my blood sugar is so and so, tell them how much I have had to eat, and ask how much insulin to take” (diabetic child). “I joined a network for parents of diabetics, and we got most of our knowledge about food, daily life, shopping, inspiration, and friends from it” (parent of teen diabetic).
Another central activity is remembering, e.g., remembering to take medicine: “When I am busy at work, I often lose control. My blood sugar gets high, and then, I cannot think” (adult diabetic). Planning is a major activity: “I do a lot of planning. We like to walk, but we have to consider not walking too far. There must be enough food nearby, and if not, we have to bring food and rest… it is very difficult to go on just a short walk” (adult diabetic). “It is very difficult to stick to a diet and, at the same time, actively participate in all the meetings I currently have at work. I definitely need help with that” (adult diabetic). Finding is also a major activity, including finding good supermarkets, restaurants, cooking information, and forms of exercise. It also includes finding people who can be trusted in specific places and finding places that make it possible to participate in public life. Informing others, e.g., colleagues, those at school and friends about the illness is an ongoing activity for diabetic families: “I would like a CD or website for schools, day-care institutions and workplaces that informs them about diabetes and what they must pay attention to” (parent of diabetic). Some of the participants revealed that they hide their illness from employers because employers are often not knowledgeable and wrongly suppose that diabetics will take too many sick days. Participants mentioned several types of stigma related to the illness. For example, people in public tend to think that a diabetic is drunk when, in fact, the diabetic is in severe need of help because of hypoglycaemia. Some diabetics had met people who wrongly supposed diabetes to be a self-caused illness: “When I was diagnosed as diabetic, some of my friends said that I could just lose weight. That was not very supportive” (adult diabetic). To illustrate this, Figure 3 places calculation in the centre of the diabetes triangle. The dotted line represents the related activities that were found to be equally important subtasks related to everyday living with diabetes via the qualitative inquiry: finding, co-operating, remembering, planning and informing.
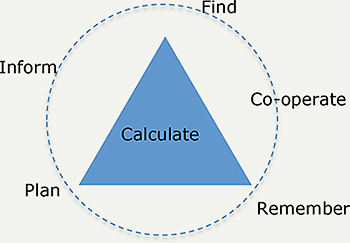
Figure 3. Activities related to diabetes practice.
These activities extend the existing literature’s investigation of the variety of tasks related to living with chronic illness (Bandura, 1984; Corbin & Strauss, 1988) and the need for technology design that works across the boundary between illness and everyday life (Aarhus & Ballegaard, 2010; Danholt, 2008; Mamykina,et al., 2006; Mullaney et al., 2012; Pullin, 2009). The core tensions between chronic illness and everyday life were derived from the analysis. These included the tensions between medical ideals and everyday practice and between the individual diabetic and their interactions within society. The tensions between medical ideals and everyday living were central to the examples of complex calculations at restaurants, difficulties in sticking to a diet at work and the complex estimations of energy use based on weather forecasts that must be performed when preparing a packed lunch for a diabetic child. The efforts required to find, plan and remember relate to the boundary work between chronic illness and everyday life. The tensions between the traditional ideal of individual self-management and the reality of social interactions were a focal point in the families’ extensive co-operation. These fundamental tensions constitute the design landscape of digital diabetes practice, as visualised in Figure 4.
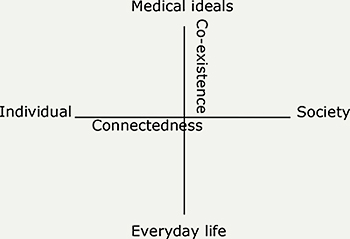
Figure 4. Core tensions in diabetes practice.
Studies of how people experience living with a chronic condition show that they typically feel healthy (Lindsey, 1996). When expressing how it feels to be healthy, they report central themes such as honouring the self, being connected with others, creating opportunities and celebrating life. Studies like these support an understanding of health and illness as co-existent. Consequently, a focus on illness, as is found in traditional diabetes technologies, will indicate that, “a large part of a person’s whole is missing and therefore denied” (Lindsey, 1996, p. 466). A focus on co-existence when balancing the vertical axis of the design landscape is central. Design research on impairment supports this need for co-existence, but it also emphasises society’s responsibility to engage in design that includes people suffering from disability and illness: “In the context of an environment or society that takes little or no account of impairment, people’s activities can be limited and their social participation restricted. People are disabled by the society they live in, not directly by their impairment” (Pullin, 2009, p. 2). Designing for health calls for a focus on supporting people’s ability to connect with others because its opposite, illness, often makes them conscious of the disconnection and isolation that come from a sense of unhealthiness. Thus, a focus on connectedness when balancing the horizontal axis of the design landscape is central. Figure 4 illustrates the core tensions and foci of balance.
Designing for Diabetes Practice
The maXi-project explored a series of prototypes within this design landscape (Figure 4) in a living laboratory set-up for the occasion over a total of four weekends in the city of Skagen, Denmark. The 17 families resided in holiday cottages for a weekend and participated in a scheduled program of everyday life activities, including grocery shopping, family lunches, walking tours, restaurant visits etc. (cf. Figure 3). Living lab experiments were set-up in close co-operation with service providers in the city to simulate and explore digital support for everyday living with diabetes (Kanstrup, Bjerge, & Kristensen, 2010). The role of the digital prototypes was to enable design reflections through exploring the design space, that is, prototypes were used for “traversing a design space, leading to the creation of meaningful knowledge about the final design” (Lim, Stolterman, & Tanenberg, 2008, p. 3). The digital prototypes functioned as “technology probes” (Hutchinson et al., 2003) to explore possible directions within the design landscape of everyday living with diabetes. This probing process embraced “probology”, “an approach that uses probes to encourage subjective engagement, empathetic interpretation, and a pervasive sense of uncertainty as positive values for design” (Gaver, Boucher, Pennington, & Walker, 2004, p. 56). The following prototypes were explored:
MaXine: This prototype focused on simulating blood glucose level. Personal data are entered into an algorithm. The prototype is designed for a personal computer and uses drag-and-drop interaction; food, insulin doses and exercise are dragged from the top menu and dropped into a timeline. The effect of the chosen action on glucose level is visualized immediately via a curve in the timeline in the main interface of the prototype.
To highlight the exploratory character of the prototype, the user interface was sketchy, with home-made icons representing food, medicine, a bicycle, running shoes and a glucose meter.
The simulation provided by the MaXine prototype is not precise and cannot be trusted blindly. It was developed because all participants in the design project expressed the dream of being able to glimpse their future glucose levels. Despite its inaccuracy, such a simulation could be used to support informed guessing. The participants explained how they typically make guesses about their future glucose levels on the basis of the weather forecast, continual planning or co-operation for example.
Wild rabbits: This prototype supported the sharing of information about food. It is a database containing information about food, service providers, comments and rankings. Information can be viewed, added, modified and related to text comments on experiences, tips and ratings. Users interact with the database through an iPhone application that has search functions for specific types of food or service providers. More than 400 food products were entered into the prototype, along with basic information about the energy, protein, fat and carbohydrates they contain. Information is accessed by searching the database or via barcode scanning using the iPhone camera. The Wild rabbit prototype was designed because the participants emphasised the importance of sharing their experiences with food and service providers. In the interviews and workshops, participants had described printed information as difficult to access and decode and advice from other diabetics as valuable. For this reason, the prototype was developed to help users explore detailed product information and user experience information.
Two prototypes focused on providing information from service providers regarding ingredients in unlabelled food. Location-based health services were installed at a butcher’s shop. Information on selected types of food was provided on a screen in the shop via RFID tags and USB readers. Mobile health services were installed at a restaurant where QR tags taped to the menu provided access to recipes via a mobile phone. Information about ingredients in bread, accessed via a mobile phone, was explored in bakeries. These prototypes were developed and explored because of the participants’ problems in finding information about unlabelled food. The participating service providers offered information via text and photos about the ingredients of products.
Social Learning Theory and the Notion of Practice
The social learning theory of situated learning and communities of practice (CoPs) presented by Lave and Wenger (1991) and Wenger (1998) has worked as a theoretical framework for analysing data from the design process and creating design concepts for digital diabetes practice. This theory’s attention to social practice, as opposed to a series of tasks related to self-management, supports the understanding of diabetes as a complex practice of multiple interactions, as opposed to an object to be managed by the individual. A CoP pays attention to the dynamics and diversities in a given practice, these being central to understanding the tensions in everyday life with diabetes. Lave and Wengers’ concept of legitimate peripheral participation (LPP) provides a developmental understanding of practice as opposed to fixed categories of “diabetics” and “diabetes tasks”.
The concept of a CoP is defined by a combination of i) people being connected by a domain of shared interests, uniting members in active sharing and the development of interests; ii) members’ active engagement in joint activities and negotiations; and iii) an active practice, along with the ongoing development of a shared repertoire of experiences, tools, language and approaches. A CoP allows for, but does not assume, intentionality. Wenger outlines this definition in terms of three dimensions by which practice is the source of coherence within a community: mutual engagement, joint enterprise and shared repertoire (Wenger, 1998, pp. 72-73). These are all positive terms and point to the understanding of a CoP as a “locus of engagement in action, interpersonal relations, shared knowledge, and negotiation of enterprises” and as a possible platform for “real transformation” (Wenger, 1998, p. 85). These dimensions are characterized not by their agreements, but by participation and diversity. Mutual engagement entails being included and engaging oneself in activities in order to define belonging within a practice. This dimension emphasises the active work participants must do (Wenger, 1998, pp. 73-74). Mutual engagement is characterised by diversity and is partial: “it draws on our ability to connect to others’ knowledge and contribution” (Wenger, 1998, pp. 75-76). When mutual engagement is sustained, it connects participants within CoPs (Wenger, 1998, pp. 76-77). Joint enterprise is characterised as the result of a collective process of negotiation (Wenger 1998, pp. 77-78). Again, agreement is not required. Rather, disagreement can be viewed as productive. Negotiation is central, as are conditions, resources and demands—what matters and what does not can only shape practice when negotiated by a community (Wenger, 1998, pp. 79-82). Shared repertoires include routines, words, tools, ways of doing things, stories, etc. (Wenger, 1998, pp. 82-83).
LPP is a concept that situates participants’ learning as part of a CoP. The mastery of knowledge and skills is obtained via participants’ movements within a CoP, typically from a peripheral position, as a newcomer in a CoP, toward full participation (Lave & Wenger, 1999, p. 83). This focus on participants’ movements brings attention to trajectory. LPP is not a linear, step-wise process from a participant’s initially peripheral position in a CoP towards full membership. Rather, LPP’s focus on trajectory brings the complex movements and interactions of participants and practices to the foreground. Lave and Wenger (1999, p. 87) emphasize there is no such thing as an “illegitimate peripheral participant”. Similarly, there is no such thing as “central participation” in a CoP. On the contrary, “changing locations and perspectives are part of actors’ learning trajectories, developing identities, and forms of membership” (Lave & Wenger, 1999, p. 87). Peripherality and legitimacy are types of modification that are required to make participation possible. These are positive perspectives on participation. Peripheral participation suggests an opening that may lead to more intensive participation. Legitimacy emphasises the inclusiveness required for participation. Wenger elaborates on these concepts as follows (Wenger, 1998, pp. 100-101): Peripherality provides an approximation of full participation. He emphasises that “No matter how the peripherality of initial participation is achieved, it must engage newcomers and provide a sense of how the community operates.” Only people who are members of the community can participate and play a role. The acknowledgement that peripheral participation can take many forms is central. Wenger emphasises that newcomers can only be on an inbound trajectory if they are granted enough legitimacy to be treated as potential members: “Granting the newcomers legitimacy is important because they are likely to come short of what the community regard as competent engagement. Only with enough legitimacy can all their inevitable stumblings and violations become opportunities for learning rather than cause for dismissal, neglect, or exclusion”. Legitimacy can take many forms. Peripherality and legitimacy are not free of conflicts. Working out perspectives involves “a dynamic of continuity and discontinuity that propels the practice forward” (Wenger, 1998, p. 101).
The notion of practice involving on going dynamic interactions and divergent negotiations extends our understanding of design for digital diabetes practice to include support for mutual engagement (participants’ active participation and connections), joint enterprise (participants’ negotiations of meaning) and shared repertoire (participants’ (re)-development of language, tools, routines, etc.), with a focus on obtaining legitimacy through participation (engaging, including and supporting increased participation). This perspective on practice operated as the theoretical framework during the analysis of the living lab experiments.
Emerging Design Concepts
The core concepts from the theoretical framework—mutual engagement, joint enterprise, shared repertoire and legitimate peripheral participation—were applied in the analysis of the data from the living lab experiments. This data included diaries written by each family over the weekend, interviews carried out with the participants after each experiment and a concluding design workshop in which the experiences were summed up and the families contributed design ideas for digital diabetes practice (Kanstrup 2012; Kanstrup, 2013). The data were transcribed and coded in relation to the theoretical framework. From this analysis, three design concepts emerged as central to the design of digital diabetes practice. The design concepts are independent, but compose a comprehensive unity of design for digital diabetes practice.
Explore Chronic Illness—Learning Diabetes
The MaXine prototype (Figure 5) was introduced to the participating families on their first day in the living lab. They used the prototype over the weekend, inserting data on food, exercise and medication, and evaluated its impact in the concluding workshop. The results from the MaXine prototype pointed to the importance of learning the shared repertoire, that is, the basic curriculum of diabetes and the basic actions and tools related to the illness in a fun and engaging way. MaXine supported participants in exploring the dynamics of the elements of the diabetes triangle (Figure 2) and learning about the diabetes vocabulary, dynamics, dangers and possible actions in a safe way.
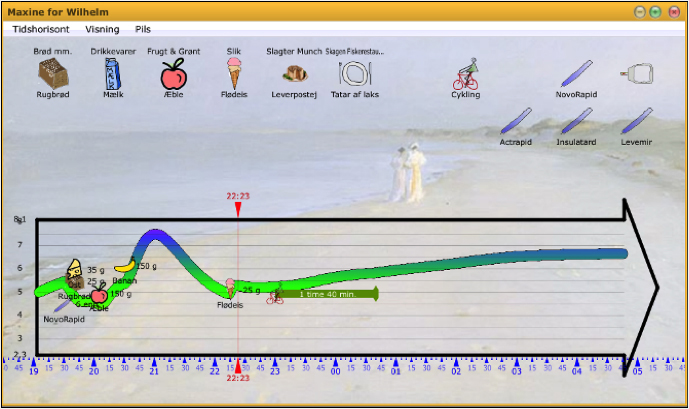
Figure 5. Primary user interface of the MaXine prototype.
The diabetes curriculum is complex. It begins in the body, but moves quickly out of the body and into core everyday activities related to the illness (Figure 3). The movement from understanding the body to understanding how to perform diabetes in everyday life requires experience-based learning.
The MaXine prototype aims to support such learning by providing a safe zone for simulating real-life activities. Actions, emotions, dreams and fears can be explored and supported via conversations among participants engaged in interaction with the digital prototype.
The newcomer learns by joining and participating. One central factor to this prototype was its ability to enrol participants via co-operative ludic explorations of possible ways of performing diabetes. Legitimacy is obtained via participation. One cannot perform wrongly—the consequences of actions are only simulated and breaking the rules can even be fun. For example, two of the diabetic children in the design project wanted to explore extreme situations (e.g., their fears) and inserted only what they called “wild actions” into the MaXine prototype, such as biking for 24 hours, eating five kilos of apples, injecting double doses of insulin, etc. This elicited a laugh from the children and attracted participants.
The design concept of exploring chronic illness emerged from these results. In contrast to medical perspectives focused on body counts, evidence and reality, the concept of exploring is not related to facts. It is related to leaving the body and everyday reality to explore the dynamics of a given illness in a fun and engaging way.
Exploration requires safe gear. Digital health services focused on exploring chronic illness must provide a safe zone, just as a sandbox provides a safe zone for kids to explore through play.
Exploration requires curiosity and investigation. Digital health services focused on exploring chronic illness must provide materials that are tangible and ludic and provide instant feedback on explorations.
Participants join for the experience. Digital health services focused on exploring chronic illness must support memorable experiences, language, actions, tools and a shared repertoire of use for participation in diabetes practice.
Share Chronic Illnesss—Negotiating Doing Being a Diabetic
The Wild rabbit prototype (Figure 6) was introduced to the participating families on their first day in the living lab (Friday). They were free to try out the iPhone application over the entire weekend and were asked to participate in experiments set-up at i) a supermarket where they did grocery shopping; ii) two bakeries where they went for breakfast; and iii) restaurants where they had dinner. The participants were able to access information from service providers and other participants, and they were able to add information to the prototype. The prototype was evaluated during the concluding workshop. One clear result of these experiments was that information from service providers was not deemed to be particularly important. Instead, the participants’ own production and sharing of experiences were emphasised as being valuable. The participants requested more digital support for active negotiations on their own part. Having a social pattern to follow that consists of others’ experiences is fine, but the negotiation of social patterns was pointed out as having real value.
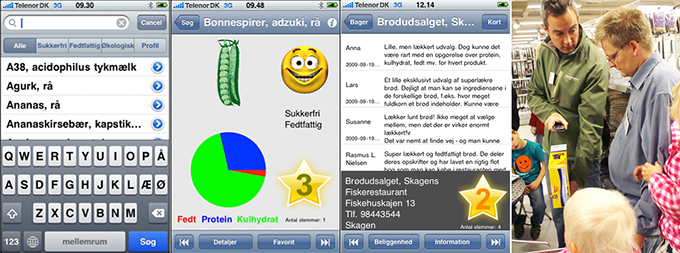
Figure 6. Primary user interfaces of the wild rabbit prototype.
Photo one: search in the database.
Photo two: information on food and ratings from participants shown in the star.
Photo three: shared information on restaurants. Photo four: barcode scanning in the supermarket.
The design concept of sharing chronic illness emerged from these results. In contrast to medical perspectives focused on the individual self-management of health data, the concept of sharing is collaborative and qualitative. Sharing calls for a CoP. Digital health services that support sharing must provide a platform for a CoP, which supports active participation, mutual engagement, joint enterprise and a shared repertoire as a basis for negotiating meaning in practice among participants.
Negotiations are crucial to the concept of sharing. Digital health services aimed at supporting people in sharing chronic illness must support negotiations of meaning among participants, which is more than mere links and “likes”.
Participants join together to negotiate meaning. They define who they are by the way they experience themselves through participation and by the ways they and others reify themselves in social patterns. Wenger (1998, p. 149) writes, “There is a profound connection between identity and practice. Developing a practice requires the formation of a community whose members can engage with one another and thus acknowledge each other as participants. As a consequence, a practice entails the negotiation of ways of being a person in that context”. The Wild rabbit prototype emphasised the importance of supporting participants’ negotiations of the “ways of being a person in that context” (Wenger, 1998, p. 149). Ethnomethodologist Harvey Sacks (1984, p. 415), writing about the relationship between doing and being, coined the phrase “doing being”, which has been an additional theoretical inspiration in this analysis. “Doing being” refers to the way “somebody constitutes oneself, and, in effect, a job that persons and the people around them may be coordinatively engaged in”. Digital diabetes designs must support this coordinative engagement in doing being a diabetic by supporting people in their on going constitution of themselves as persons affected with a chronic illness.
Camouflage Chronic Illnesss—Mastering Multi-membership
Location-based and mobile health services (Figure 7) were set-up at various service providers, including a butcher’s shop, two bakeries, and four restaurants. On the second and third day of the living lab (Saturday and Sunday), the participants were asked to explore the prototypes via grocery shopping and dining. The participants were prompted to use the prototype to find information before buying bread and cold meat for breakfast and lunch and before ordering food at restaurants. The prototype was evaluated in the concluding workshop. The results from this exploration of location-based and mobile health services brought attention to the need for identity support, which can be difficult as a diabetic (Corbin & Strauss, 1988). An example from the design project shows how a lack of experience and the loss of identity can make people feel as if they stand out during activities that were previously ordinary, such as grocery shopping: “I hate these shelves in the supermarket with diet and sugar-free food. I feel that everybody can see that I am diabetic when I stand in front of these shelves. I want to move around in the supermarket like I used to do before I was diagnosed with diabetes” (diabetic adult). For this reason, participants called for design solutions that were integrated into mobile phones: “I like that no one can see what I am looking for with the mobile phone because they cannot tell whether it is a text message, a shopping list, or information about carbohydrates” (diabetic adult).

Figure 7. Participants exploring location-based health services with RFID readers in a butcher’s shop (left photo), with QR tags on the menu at a restaurant (middle photo), and via mobile health services at a bakery (right photo).
Another central statement related to diabetes and identity is “I say, ‘I am Anna’. I don’t say, ‘I am diabetic’” (diabetic teenager). Anna spends resources every day to hide her diabetes. The following quote exemplifies how stressful a city tour with friends can be: “If I am in the city with my friends and buy a piece of chocolate, it is difficult to find a place where I can take my insulin. I won’t go into a dirty public toilet and I won’t do it in some shop behind a shelf. Sometimes, I wait, and that is not good. Then, my blood sugar becomes unstable. I get angry and use a lot of energy thinking about when I can take my insulin, and then, I have to find a toilet that is clean. The fitting rooms in the boutiques are also difficult to use because the shop assistants always come and ask if everything is fine. I use a lot of energy not to reveal that I am diabetic” (teen diabetic). In the living lab design workshop, Anna created designs that supported her identity as Anna, such as a medical devices integrated into jewellery.
Wenger (1998, p. 159) notes, “Identities are not something we turn on and off. Our various forms of participation are not merely sequences in time: Our various forms of participation delineate pieces of a puzzle we put together rather than shape boundaries between disconnected parts of ourselves. An identity is thus more than just a single trajectory; instead, it should be viewed as a nexus of multi-membership”. Anna’s design of medical devices integrated into jewellery is an example of a design supporting such multi-membership (Kanstrup, 2013). The design concept of camouflage emerged from these results. In contrast to medical perspectives placing illness in the foreground, the concept of camouflage aims to blur and blend. It moves the focus from illness to identity, including issues such as fashion (Kanstrup, 2013) and emotions (Glasemann & Kanstrup, 2011).
Camouflage focuses on the ability to blend in and design digital health services intended to undo social stigma. Goffman’s (1963) concept of “passing” to avoid social stigma has been an additional theoretical inspiration for this analysis. Goffman describes how the phenomenon of passing is observed when a stigma is not directly observable to others. According to Goffman, individuals at risk of social stigma learn to pass. An example is how blind people learn to aim their eyes directly at the person they are talking to. Being in control of identity information is crucial for passing. Two often-used strategies are to either remove the signs of stigma or to present the signs of stigma as signs of other attributes. This is what Anna does when she suggests integrating blood glucose meters into jewellery. The signs of diabetes are transformed to the signs of fashion.
Camouflage supports of the ability to master identity and multi-membership. This calls for digital health services aimed at supporting people in their attempt to remain in control of identity information. Participants use camouflage to support themselves in participation, that is, digital health services focused on camouflage must be designed to support legitimacy and membership in concrete situations, in contrast to neglect or exclusion.
Temporal and Spatial Dimensions of the Design Concepts
The differences between the supplementary aspects of the three design concepts become apparent when examining their temporal aspects:
- Exploring looks forward to possible futures and considers what might happen if certain decisions are taken. It is related to the temporal aspect of LPP in that participants can obtain legitimacy by moving from the periphery towards increased participation. It is related to the shared repertoire of a CoP developed by the participants while exploring their chronic illness. Exploring provides peripheral access to future actions.
- Sharing looks back on actions that are worth repeating. It is related to the negotiation of meanings, the development of mutual engagement, and a shared repertoire of CoP via the sharing of selected actions. Sharing supports negotiations regarding past actions.
- Camouflage is focused on the present. It is related to the need for legitimacy in concrete situations and the ability to obtain multi-membership. Camouflage provides the diabetic with legitimacy in situ.
Also, the differences between and supplementary spatial aspects of the three design concepts are important:
- Exploring is seeking out possible actions. It supports the investigation of complex movements and interactions. It places the explorer in a p eripheral position with increased legitimacy, competence and participation. Exploring provides a route for increased participation.
- Sharing is rooted in concrete situations. It involves sharing concrete actions and supporting the negotiation of the joint enterprise of diabetes practice. Sharing supports spaces of joint enterprise.
- Camouflage is dually occupied with the concrete situation and identity and membership. It focuses on movements, the “changings locations and perspectives” that are “part of actors’ learning trajectories, developing identities, and forms of membership” (Lave & Wenger, 1991, p. 87). Camouflage facilitates movements between situations and identity.
In sum, the temporal and spatial differences between the design concepts should encourage designers to reflect on how to design ICTs that facilitate diabetics’ temporal and spatial movements in and out of communities of practice.
The design concepts expand the solution space of digital diabetes practice from a medically oriented position concerned with an individual’s self-management to a position that embraces the core tensions in diabetes practice (Figures 3 and 4). The design concepts facilitate users’ interactions across boundaries in their everyday lives: Exploring emphasises the important connection between medical ideals and the everyday lives that diabetes families must learn to manage. They prefer to learn in a safe zone as opposed to taking risks in public situations. This design concept is visualised as central to creating balance across the private-oriented part of the design landscape of digital diabetes practice (Figure 8). Sharing emphasises the importance of creating connections that support people in co-managing co-existence with chronic illness in public life through on going negotiations of meanings. This design concept is visualised as central to creating balance across the public-oriented part of the design landscape (Figure 8). Camouflage emphasises the importance of supporting people in blending in and “passing” in public situations so as to avoid the social stigma related to being a diabetic (Goffman, 1963). This design concept is visualised as central to creating a balance across private and public tensions in the everyday-life-oriented part of the design landscape (Figure 8).
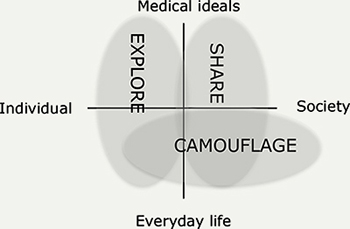
Figure 8. The three design concepts supporting interactions across tensions in everyday diabetes practice.
Conclusion
This paper has presented an analysis of research results that identify the core tensions between diabetes and everyday life activities. On this basis, three design concepts for digital diabetes practice were developed. The three design concepts are:
- Design to explore chronic illness: this concept encourages designers to support playful learning in a safe zone, which requires tangible, ludic materials, along with safe exploration and feedback.
- Design to share chronic illness: this concept encourages designers to support the negotiation of doing being diabetic. It requires a platform for a community of practice that supports negotiations regarding the co-existence of illness and the realities of everyday life.
- Design to camouflage chronic illness: this concept encourages designers to support the mastery of identity and multi-membership, which requires the ability to blend in, support legitimacy and remain in control of identity information.
The design concepts are not exhaustive in terms of design for digital diabetes practice. However, being rooted in long-term empirical studies and conceptualised on the basis of a theoretical framework for understanding practice, they provide a grounded point of departure for designers entering the field of digital design for chronic illness. In sum, the design concepts present a holistic perspective on digital diabetes practice supporting engagement in a broad set of everyday problems related to diabetes. Working on several dimensions at once requires broad design skills. A designer’s ability to navigate and reflect on positions within this broad landscape of diabetes practice is important. The three design concepts offer this opportunity.
Why design concepts? Buchanan (1995) argues that re-positioning is fundamental in order to escape habitual placements within design. According to Buchanan, the systematic pattern of invention within design is “found not in a set of categories but in a rich, diverse, and changing set of placements”. Buchanan uses the term placements to refer to conceptual perspectives, that is, as a synonym for the term “design concepts” used in this paper. In this paper, the term design concept is used to emphasize the conceptual characteristics of design synthesis. Design concepts are not prescriptions or instructions, but rather conceptual tools for re-thinking digital diabetes support. Design concepts are not predefined ways of approaching reality, but rather useful inspirational tools that can be incorporated into specific processes and situations by the designer (Stolterman, 2008) to prepare the designer for action (Schön, 1983). As explained by Buchanan (1995), design concepts offer “placements” to designers: “placements … are not rigidly fixed and determinate. The boundary of a placement guides a context or orientation to thinking (…). Therefore, placements are sources of new ideas and possibilities when applied to problems in concrete circumstances” (pp. 10-11). The three design concepts presented in this paper offer positions to systematically work with in the invention of digital diabetes technology.
The design concepts can also be used as analytic tools. The explore concept can be used for the analysis of existing learning technologies for diabetics. How do learning technologies for diabetics support the exploration of possible actions in a fun and engaging manner within a digital safe-zone? The sharing concept can be used to analyse the wealth of social networking technologies in which people with chronic illnesses support one another virtually. These technologies are characterised by being focused on emphatic communication (Preece, 1998), but how do they support the negotiation of meanings on being a diabetic? The concept of camouflage can work as an excellent analytic tool for analysing public technologies. How do price scanners in supermarkets, mobile services, etc. facilitate legitimacy for the diabetic in situ?
The related work and empirical results from the presented design research study stress a need for innovative technologies to support everyday living with chronic illness. The concepts explore, share and camouflage are important qualities to digital design for diabetes practice.
Acknowledgments
The Danish Business Authority and the Faculty of Humanities at Aalborg University supported this research. Thanks to all participants; The Danish Technological Institute, The Foundation of Skagen Wellness, Edvantage Group and project research colleagues Pernille Bertelsen, Christian Nøhr and Marie Glasemann. A special thanks to the 17 families and the 9 service providers who participated in the living lab experiments.
References
- Aarhus, R., & Ballegaard, S. A. (2010). Negotiating boundaries: Managing disease at home. In E. Mynatt, G. Fitzpatrick, S. Hudson, K. Edwards, & T. Rodden (Eds.), Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (pp. 1223-1232). New York, NY: ACM.
- Bandura, A. (1984). Recycling misconceptions of perceived self-efficacy. Cognitive Therapy and Research, 8(3), 231-255.
- Bandura, A. (1977). Self-efficacy: Towards a unifying theory of behavioral change. Psychological Review, 84(2), 191-215.
- Boisen, E., Bygholm, A., Cavan, D., & Hejlesen, O. (2003). Copability, coping, and learning as focal concepts in the evaluation of computerised diabetes disease management. International Journal of Medical Informatics, 70(2-3), 353-363.
- Brandt, E. (2006). Designing exploratory design games: A framework for participation in participatory design? In G. Jacucci & F. Kensing (Eds.), Proceedings of the 9th Conference on Participatory Design: Expanding Boundaries in Design (Vol. 1, pp. 57-66). New York, NY: ACM.
- Brandt, E., Messeter, J., & Binder, T. (2008). Formatting design dialogues – Games and participation. CoDesign, 4(1), 51-64.
- Buchanan, R. (1995). Wicked problems in design thinking. In V. Margolin & R. Buchanan (Eds.), The idea of design (pp. 3-20). Cambridge, UK: MIT Press.
- Buxton, B. (2010). Sketching user experiences: Getting the design right and the right design. San Francisco, CA: Morgan Kaufmann.
- Corbin, J., & Strauss, A. (1988). Unending work and care: Managing chronic illness at home. San Francisco, CA: Jossey-Bass.
- Danholt, P. (2008). Interacting bodies: Posthuman enactments of the problem of diabetes – Relating science. (Doctoral dissertation). Roskilde University, Roskilde, Denmark.
- Gaver, W. W., Boucher, A., Pennington, S., & Walker, B. (2004). Cultural probes and the value of uncertainty. Interactions, 11(5), 53-56.
- Glasemann, M., & Kanstrup, A. M. (2011). Emotions on diabetes: A design case of user mock-ups by young living with diabetes. CoDesign, 7(2), 123-130.
- Glasemann, M., Kanstrup, A. M., & Ryberg, T. (2010) Making chocolate-covered broccoli: Designing a mobile learning game about food for young people with diabetes. In O. W. Bertelsen, P. Krogh, K. Halskov, & M. G. Petersen (Eds.), Proceedings of the 8th ACM Conference on Designing Interactive Systems (pp. 262-271). New York, NY: ACM.
- Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. London, UK: Penguin Books.
- Greenbaum, J., & Kyng, M. (1991). Design at work: Co-operative design of computer systems. Hillsdale, NJ: Lawrence Erlbaum Associates.
- Hutchinson, H., Mackay, W., Westerlund, B., Bederson, B. B., Druin, A., Plaisant, C., … & Eiderbäck, B. (2003). Technology probes: Inspiring design for and with families. In G. Cockton & P. Korhonen (Eds.), Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (pp. 17-24). New York, NY: ACM.
- Kanstrup, A. M. (2012). A small matter of design: an analysis of end users as designers. In K, Halskov, H. Winschiers-Theophilus, Y. Lee, J. Simonsen, & K. Bødker (Eds.), Proceedings of the 12th Conference on Participatory Design (Vol. 1, pp. 109-118). New York, NY: ACM..
- Kanstrup, A. M. (2013). Designed by end users: Meanings of technology in the case of everyday life with diabetes. End-User Development: Lecture Notes in Computer Science, 7897, 185-200.
- Kanstrup, A. M., & Bertelsen, P. (2011). User innovation management: A handbook. Aalborg, Denmark: Aalborg University Press.
- Kanstrup, A. M., Bjerge, K., & Kristensen, J. (2010). A living laboratory exploring mobile support for everyday life with diabetes. Wireless Personal Communications, 53(3), 395-408.
- Kanstrup, A. M., Bertelsen, P., Glasemann, M., & Boye, N. (2008). Design for more: An ambient perspective on diabetes. In D. Hakken, J., Simonsen, & T. Robertson (Eds.), Proceedings of the 10th Anniversary Conference on Participatory Design (pp. 118-127). New York, NY: ACM.
- Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. Cambridge, UK: Cambridge University Press.
- Lave, J., & Wenger, E. (1999). Legitimate peripheral participation. In P. Murphy (Ed.), Learners, learning and assessment. London, UK: Paul Chapman Publishing.
- Lim, Y. K., Stolterman, E., & Tanenberg, J. (2008). The anatomy of prototypes: Prototypes as filters, prototypes as manifestations of design ideas. ACM Transactions on Computer-Human Interaction, 15(2), 7.
- Lindsey, E. (1996). Health within illness: Experiences of chronically ill/disabled people. Journal of Advanced Nursing, 24(3), 465-472.
- Lorig, K., & Holman, H. (2003). Self-management education: History, definitions, outcomes, and mechanisms. Annals of Behavioral Medicine, 26(1), 1-7.
- Mamykina, L., Mynatt, E., & Kaufman, D. (2006). Investigating health management practices of individuals with diabetes. In R. Grinter, T. Rodden, P. Aoki, E. Cutrell, R. Jeffries, & G. Olson (Eds), Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (pp. 927-936). New York, NY: ACM.
- Mukherjee, N. (2002). Participatory learning and action: With 100 field methods. New Delhi, India: Concept Publishing.
- Mullaney, T., Petterson, H., Nyholm, T., & Stolterman, E. (2012). Thinking beyond the cure : A case for human-centered design in cancer care. International Journal of Design, 6(3), 27-39.
- Newell, A. F., P. Gregor, M., Morgan, G. P., & Macaulay, C. (2011). User-sensitive inclusive design. Universal Access in the Information Society, 10(3), 235-243.
- Papanek, V. (1984). Design for the real world. Human ecology and social change. London, UK: Thames & Hudson.
- Preece, J. (1998). Empathic communities: Reaching out across the web. Interactions, 5(2), 32-43.
- Pullin, G. (2009). Design meets disability. Cambridge, MA: MIT Press.
- Robertson, T., & Simonsen, J. (2012). Challenges and opportunities in contemporary participatory design. Design Issues, 28(3), 3-9.
- Sacks, H. (1984). On doing “being ordinary”. In J. Atkinson & J. Heritage (Eds.), Structures of social action: Studies in conversation analysis (pp. 413-429). Cambridge, UK: Cambridge University Press.
- Schön, D. A. (1983). The reflective practitioner: How professionals think in action. New York, NY: Basic Books.
- Stolterman, E. (2008). The nature of design practice and implications for interaction design research. International Journal of Design, 2(1), 55-65.
- Wenger, E. (1998). Communities of practice: Learning, meaning, and identity. Cambridge, UK: Cambridge University Press.

